Colon And Rectal Surgery
What is the
Colon and Rectum?
The colon and rectum together form the large intestines. The last 15cm of the large intestines is known as the rectum, while the rest of it is called the colon. This is the last part of the digestive system. The small intestine is responsible for most of the digestion of food and absorption of nutrients. Whatever that is not absorbed passes into the colon, where most of the water is absorbed by the body.
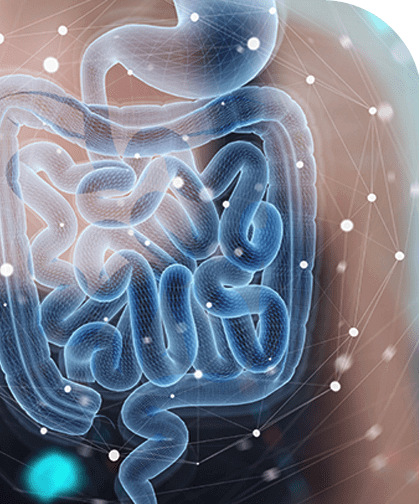
What Conditions
Require Colon
and Rectum Surgery?
Majority of the colon and rectum surgery done in Singapore are for colon and rectal cancer. Less frequently, they
are performed for conditions such as diverticular disease, ulcerative colitis, Crohn’s disease, chronic constipation
or rectal prolapse.
Colon surgery is almost always performed through the abdomen. In suitable cases of rectal surgery, the surgery is
performed through the anus.
What is Done at the Time of Surgery?
Most colon and rectum surgery entails removing a portion of the colon or rectum. In the majority of
cases, the 2 cut ends are then joined back together to restore continuity to the intestines. This restores normal
bowel function.
The segment of colon or rectum to be removed is determined by the location of the disease. The blood
vessels that supply this segment are first cut off. If the surgery is for cancer, particular attention would be paid
to remove the lymph nodes that run along these vessels.
Removal of part of the colon is referred to as a colectomy. Numerous names of surgery are used to
describe the portion of the colon that is removed, such as right hemicolectomy (removing right half of the colon),
left hemicolectomy (removing left half of colon), total colectomy (removing the entire colon) and sigmoid colectomy
(removing the sigmoid colon). For surgery involving the rectum, the term proctectomy or anterior resection is used.
Is a Stoma Always Necessary?
NO. Most operations do not require a stoma.
When is a Stoma Necessary?
In cases of cancer of the rectum or anus where the anus sphincter muscles are involved, removing the
cancer would require the anal muscles to be sacrificed. Under such circumstance, there would not be any muscles left
to prevent the stools from leaking out. In these patients, a permanent stoma would be necessary. This is required in
less than 5% of colorectal surgery.
In some cases of rectal surgery, when the anastomosis (joint between the 2 ends of the colon/rectum) is
very near the anus, it is well established that the blood supply there is poor and there is a higher risk of the joint
not healing and giving way. By having a stoma, this diverts the faeces out through the abdomen and prevents it from
coming through the joint. This allows the anastomosis time to heal properly without risk of leakage of faecal content.
These stomas are temporary and are usually closed 1-2 months later when the anastomosis has confirmed to be healed.
How is Colon and Rectum Surgery Performed?
There have been many improvements in the surgical instruments and techniques over the last 15 years.
The standard conventional surgery has always been through a long vertical cut through the abdomen in
order to access the organs within. As this cut is relatively long, the post-operative pain can be quite substantial
and recovery could be slow.
With improved techniques, some surgeons went on to make a horizontal cut in the lower part of the
abdomen to remove the specific colon and rectum. This results in less pain than a long vertical cut.
With the advancement of technology, minimally invasive colon and rectum surgery is now becoming more and more common.
Minimally Invasive Colon and Rectum Surgery
Standard Laparoscopic Colorectal Surgery
The colon and rectum are approached using thin and long instruments instead of making a long open cut.
A 1cm cut is made at the umbilicus and the camera is inserted. Three or four other cuts of 5-10mm is
made around the abdomen. This allows instruments to be inserted inside and manipulate the intestines to perform the
surgery. One of these cuts is then enlarged to allow the resected colon to be removed from the body.
Single Incision Laparoscopic Colorectal Surgery
With better instruments, we have now moved on to single incision laparoscopic port surgery. This means that instead of having 3-5 small incisions around the abdomen, all the instruments are inserted through a special device that is usually located at the umbilicus. The colon is also removed through the same cut.
Robotic Colorectal Surgery
The latest advancement in technology is robotic surgery. Robotic surgery is also a form of minimally invasive surgery.
Likewise, it utilises a few small holes that are made in the abdominal wall. However, unlike standard laparoscopic
surgery where a few straight instruments are inserted, fine robotic arms are inserted through these small holes to do
the surgery.
Robotic surgery gives the surgeon a 3-dimensional view and higher
magnification. This allows easier identification of the nerves and reduces the risk of damage. The flexibility of the
instruments is also much better compared to the standard laparoscopic instruments.
The difference between robotic and standard laparoscopic instrument is almost like using your hands compared to using
a pair of chopsticks. It also allows for easier surgery deep in the pelvis within the confines of the pelvic bones. In
certain cases, this improvement might make the difference between preserving the anus and having a permanent stoma.
Advantages of Minimally Invasive Surgery
With a smaller incision, there is usually less pain and allows the patient to be up and about more quickly. This may or may not result in a shorter hospital stay as that depends on the individual patient. However, with minimally invasive surgery, the patient usually has a faster return to normal daily activities after discharge.
Step by Step Guide to Colon and Rectum Cancer Surgery
Before Surgery
As the surgery is most commonly performed under general anaesthesia, your colorectal surgeon will likely arrange for some blood
test, electrocardiogram (ECG) and chest x-rays before surgery. This is to ensure that you are fit for surgery. Your
anaesthetist may also see you before the surgery if required. For cancer surgery, a CT scan may also be done to give
more detailed information about the location and its extent of spread before surgery.
You will be required to fast for 6 hours before the surgery. Medication will also be given to clear the bowel of any
residual faeces. An intravenous drip may also be given to ensure adequate hydration during the period of fasting.
During Surgery
After anaesthesia, body hair over the site of surgery will be shaved off. A tube will also be inserted into the bladder to drain out the urine during surgery. Sometimes, a tube will also be inserted through the nose into the stomach to drain out the excess air and fluid in the stomach.
Immediately After Surgery
When you wake up from anaesthesia, the tubes that are inserted would be in place. Pain killers should have already been administered so there will not be much pain.
After Surgery
It is normal that the stomach and intestines stop functioning for up to 48 hours after colon and rectum surgery.
During this period, oral intake will be restricted. Pain killers will be administered via intravenous infusion.
The tube inserted into the bladder will usually be removed after two or three days when you are ready to get up and
go and pass urine on your own. The stomach tube, if inserted, is usually removed on the first or 2nd day.
As the intestine function slowly recovers, your surgeon will progress your oral intake from water to soft diet and
eventually to solid foods. Once you are able to eat and pass motion, you are ready to go home.
Upon Discharge
Please resume normal daily activities upon going home. The wound requires minimal care and it is alright even if it
gets a bit wet during a bath. You are advised to refrain from strenuous activities for one to two months after
surgery to allow the muscle wound to heal properly.
For more information about colon and rectum surgery, please visit our Singapore Colonoscopy Clinic website.
Our Other Services

Our Colorectal Surgeon
Better Care.
Constant Support.
Kindly fill up the form below and we will get back to you as soon as possible.

Colorectal Surgeon
Mount Elizabeth Medical Centre
#12-09, Singapore 228510
| Tel | : (+65) 6737 2778 |
| Fax | : (+65) 6737 2389 |
| : hokoksuncolorectal@gmail.com |
| Mon - Fri | : 9am - 1pm, 2pm - 5pm |
| Sat | : 9am - 1pm |
| Closed | : Sunday, Public Holiday |